Naive exosomes : overcoming cell therapy limitations
Potential of extracellular vesicles
Extracellular vesicles (EVs) are membrane-enclosed nano size objects excreted by all cell types. Their composition is cell-type dependent: a wide range of biomolecules such as proteins, enzymes, lipids, or nucleic acids can be found encapsulated in those particles [1]. Widely considered serving as information vectors between cells and, at a greater range, organs, EVs are active players participating in homeostasis and disease, acting as biological effectors in many physiological processes such as immune response, pregnancy, coagulation, and cancer. Extracellular vesicles as new therapeutic tools would allow opening a new era in cell therapy and in drug delivery. In cell therapy, by mitigating the limitations and hurdles related to the administration of viable stem cells such as the risks of uncontrolled cell replication, differentiation, or vascular occlusion.
Additionally, EVs benefit from leading advantages in terms of sterilization, storage and shelf-life compared to their cellular counterparts. In fact, many clinical trials registered at www.ClinicalTrials.gov attempt to propose an EV therapy as an alternative to a cellular therapy. For drug delivery, EVs have proven a huge potential for precise targeted delivery, paving the way for precision medicine. Because of all these properties, the EV use in therapy is supported by a growing research field. There are two main approaches in using EVs as therapeutic agents: using them as they are excreted by unmodified cells and engineering them or the producer cells.
Regenerative and immunomudalotory properties
Unmodified EVs can be used for their immune-modulatory properties and in regenerative medicine. Mesenchymal stem cells’ (MSCs) EVs are the most investigated type for those applications. Historically, MSCs were widely studied as they exhibit, when injected in animal models, very interesting immune-modulating and regenerative activities.
Essential processes in regenerative medicine are cell viability, immune responses, extracellular matrix interaction and angiogenesis. To explain tissue regeneration after the injection of MSCs in any injured organ, it was first hypothesized that MSCs would differentiate into the desired cell type to induce tissue regeneration. However, it was discovered a poor cell retention and survival in the injury site [2,3] resulting in unsatisfactory engraftment rates.
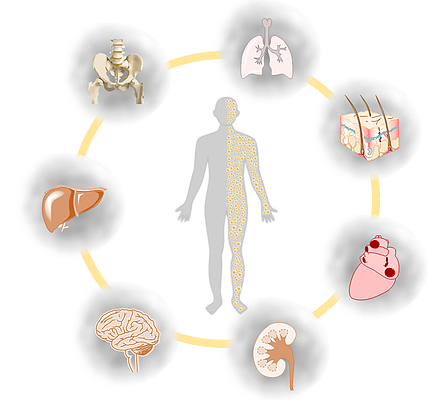
With these considerations, the second mechanism proposed is related to the cell paracrine effect mediated, amongst others, by EVs (exosomes, microvesicles and apoptotic bodies) [4,5]. Recent discoveries demonstrate that EVs generated by MSCs have protective and reparative properties to induce a regenerative effect in vivo in cardiovascular diseases, acute kidney injury, brain injury, liver injury, osteoarthritis, bone regeneration, lung injury and cutaneous wound healing [6-12]. Clinical studies on the efficacy of MSC EVs for applications in regenerative medicine are currently running (NCT05078385).
Detailed mechanism of actions
To go more in the details of the effects of EVs in regenerative processes, let’s begin with the effect on cell death and senescence. It has been demonstrated that exosomes from endothelial cells promote angiogenesis by inhibiting cellular senescence [13]. The effect has also been shown for exosomes derived from umbilical cord mesenchymal stem cells, with a suppression of apoptosis [14]: it was interestingly both demonstrated in vivo and in vitro. These protective effects seem to lead to an accelerated epithelialization in rat skin burn models [15].
Tissue regeneration requires a good local cell nutrition: angiogenesis is therefore a key milestone for the process to be successful [16]. Some results suggest MSC-derived exosomes promote angiogenesis in vitro and in vivo in rat models [17, 18]. However, EVs should be produced under hypoxic conditions to be active.
Regarding the role of EVs in extracellular matrix interaction, it has been shown that they express adhesion molecules as well as extracellular matrix remodeling proteins. Adhesion molecules such as ICAM-1, CD44, CD166 or integrins has been identified in extracellular vesicles derived from endothelial cells, dendritic cells, and reticulocytes [19, 20, 21]. As for the process of extracellular matrix remodeling, it participates in cytokine release, cell migration and angiogenesis. EVs have been shown to express proteins participating in those processes, such as matrix metalloproteinases: it is the case for cardiomyocyte progenitor cells, for example [22].
For the immune-modulatory effect, it has been shown that immune responses have a key effect on regenerative processes, allowing better recruitment, proliferation, and angiogenesis [23]. MSC EVs were demonstrated to have an immune-suppressive effect [24]. This effect was proved to be an advantaged for clinical approaches in a clinical trial using MSC derived EVs to ameliorate the progression of chronic kidney diseases [25].
For more information on translational studies employing MSC-derived microvesicles and exosomes, please refer to Donald G. Phinney et. al. (2017) [26] and Lee et. al. (2021) [27] for all the fields of application of MSC-EV based therapies.
Finally, one of the major hurdles hampering the translation of extracellular vesicles into clinical therapies is the regulatory classification of those particles, as it impacts the manufacturing and quality control requirements. Also, there are questions to be answered regarding the regulatory aspects of using products from genetically modified cells. Guidelines addressing those matters are available in Silva et al. EVOLVE review [28].
References:
[1] : Anand, S. et al. (2019) ‘Ticket to a bubble ride: Cargo sorting into exosomes and extracellular vesicles’, Biochimica et Biophysica Acta (BBA) – Proteins and Proteomics, 1867(12), p. 140203. Available at: https://doi.org/10.1016/j.bbapap.2019.02.005.
[2] : Zhang, H. et al. (2007) ‘Injection of bone marrow mesenchymal stem cells in the borderline area of infarcted myocardium: Heart status and cell distribution’, The Journal of Thoracic and Cardiovascular Surgery, 134(5), pp. 1234-1240.e1. Available at: https://doi.org/10.1016/j.jtcvs.2007.07.019.
[3] : Hale, S.L. et al. (2008) ‘Mesenchymal stem cell administration at coronary artery reperfusion in the rat by two delivery routes: A quantitative assessment’, Life Sciences, 83(13–14), pp. 511–515. Available at: https://doi.org/10.1016/j.lfs.2008.07.020.
[4] : Ratajczak, M.Z. et al. (2012) ‘Pivotal role of paracrine effects in stem cell therapies in regenerative medicine: can we translate stem cell-secreted paracrine factors and microvesicles into better therapeutic strategies?’, Leukemia, 26(6), pp. 1166–1173. Available at: https://doi.org/10.1038/leu.2011.389.
[5] : Lai, R.C., Chen, T.S. and Lim, S.K. (2011) ‘Mesenchymal stem cell exosome: a novel stem cell-based therapy for cardiovascular disease’, Regenerative Medicine, 6(4), pp. 481–492. Available at: https://doi.org/10.2217/rme.11.35.
[6] : Yuan, Y. et al. (2018) ‘Stem Cell-Derived Exosome in Cardiovascular Diseases: Macro Roles of Micro Particles’, Frontiers in Pharmacology, 9, p. 547. Available at: https://doi.org/10.3389/fphar.2018.00547.
[7] : van Koppen, A. et al. (2012) ‘Human Embryonic Mesenchymal Stem Cell-Derived Conditioned Medium Rescues Kidney Function in Rats with Established Chronic Kidney Disease’, PLoS ONE. Edited by J.-C. Dussaule, 7(6), p. e38746. Available at: https://doi.org/10.1371/journal.pone.0038746.
[8] : Xiong, Y., Mahmood, A. and Chopp, M. (2017) ‘Emerging potential of exosomes for treatment of traumatic brain injury’, Neural Regeneration Research, 12(1), p. 19. Available at: https://doi.org/10.4103/1673-5374.198966.
[9] : Cosenza, S. et al. (2017) ‘Mesenchymal stem cells derived exosomes and microparticles protect cartilage and bone from degradation in osteoarthritis’, Scientific Reports, 7(1), p. 16214. Available at: https://doi.org/10.1038/s41598-017-15376-8.
[10] : Qin, Y. et al. (2016) ‘Exosome: A Novel Approach to Stimulate Bone Regeneration through Regulation of Osteogenesis and Angiogenesis’, International Journal of Molecular Sciences, 17(5), p. 712. Available at: https://doi.org/10.3390/ijms17050712.
[11] : Willis, G.R. et al. (2020) ‘Mesenchymal stromal cell‐derived small extracellular vesicles restore lung architecture and improve exercise capacity in a model of neonatal hyperoxia‐induced lung injury’, Journal of Extracellular Vesicles, 9(1), p. 1790874. Available at: https://doi.org/10.1080/20013078.2020.1790874.
[12] : Golchin, A., Hosseinzadeh, S. and Ardeshirylajimi, A. (2018) ‘The exosomes released from different cell types and their effects in wound healing’, Journal of Cellular Biochemistry, 119(7), pp. 5043–5052. Available at: https://doi.org/10.1002/jcb.26706.
[13] : van Balkom, B.W.M. et al. (2013) ‘Endothelial cells require miR-214 to secrete exosomes that suppress senescence and induce angiogenesis in human and mouse endothelial cells’, Blood, 121(19), pp. 3997–4006. Available at: https://doi.org/10.1182/blood-2013-02-478925.
[14] : Zhang, B. et al. (2014) ‘Mesenchymal Stem Cells Secrete Immunologically Active Exosomes’, Stem Cells and Development, 23(11), pp. 1233–1244. Available at: https://doi.org/10.1089/scd.2013.0479.
[15] : Zhou, Y. et al. (2013) ‘Exosomes released by human umbilical cord mesenchymal stem cells protect against cisplatin-induced renal oxidative stress and apoptosis in vivo and in vitro’, Stem Cell Research & Therapy, 4(2), p. 34. Available at: https://doi.org/10.1186/scrt194.
[16] : Zhang, B. et al. (2015) ‘HucMSC-Exosome Mediated-Wnt4 Signaling Is Required for Cutaneous Wound Healing’, Stem Cells, 33(7), pp. 2158–2168. Available at: https://doi.org/10.1002/stem.1771.
[17] : Jain, R.K. et al. (2005) ‘Engineering vascularized tissue’, Nature Biotechnology, 23(7), pp. 821–823. Available at: https://doi.org/10.1038/nbt0705-821.
[18] : Lopatina, T. et al. (2014) ‘Platelet-derived growth factor regulates the secretion of extracellular vesicles by adipose mesenchymal stem cells and enhances their angiogenic potential’, Cell Communication and Signaling, 12(1), p. 26. Available at: https://doi.org/10.1186/1478-811X-12-26.
[19] : Bian, S. et al. (2014) ‘Extracellular vesicles derived from human bone marrow mesenchymal stem cells promote angiogenesis in a rat myocardial infarction model’, Journal of Molecular Medicine, 92(4), pp. 387–397. Available at: https://doi.org/10.1007/s00109-013-1110-5.
[20] : de Jong, O.G. et al. (2012) ‘Cellular stress conditions are reflected in the protein and RNA content of endothelial cell-derived exosomes’, Journal of Extracellular Vesicles, 1(1), p. 18396. Available at: https://doi.org/10.3402/jev.v1i0.18396.
[21] : Segura, E. et al. (2005) ‘ICAM-1 on exosomes from mature dendritic cells is critical for efficient naive T-cell priming’, Blood, 106(1), pp. 216–223. Available at: https://doi.org/10.1182/blood-2005-01-0220.
[22] : Rieu, S. et al. (2000) ‘Exosomes released during reticulocyte maturation bind to fibronectin via integrin α4β1: Integrin α4β1 is present on reticulocyte exosomes’, European Journal of Biochemistry, 267(2), pp. 583–590. Available at: https://doi.org/10.1046/j.1432-1327.2000.01036.x.
[23] : Vrijsen, K.R. et al. (2010) ‘Cardiomyocyte progenitor cell-derived exosomes stimulate migration of endothelial cells’, Journal of Cellular and Molecular Medicine, p. no-no. Available at: https://doi.org/10.1111/j.1582-4934.2010.01081.x.
[24] : Artlett, C.M. (2013) ‘Inflammasomes in wound healing and fibrosis: Inflammasomes in wound healing and fibrosis’, The Journal of Pathology, 229(2), pp. 157–167. Available at: https://doi.org/10.1002/path.4116.
[25] : Nassar, W. et al. (2016) ‘Umbilical cord mesenchymal stem cells derived extracellular vesicles can safely ameliorate the progression of chronic kidney diseases’, Biomaterials Research, 20(1), p. 21. Available at: https://doi.org/10.1186/s40824-016-0068-0.
[26] : Phinney, D.G. and Pittenger, M.F. (2017) ‘Concise Review: MSC-Derived Exosomes for Cell-Free Therapy’, Stem Cells, 35(4), pp. 851–858. Available at: https://doi.org/10.1002/stem.2575.
[27] : Lee, B.-C., Kang, I. and Yu, K.-R. (2021) ‘Therapeutic Features and Updated Clinical Trials of Mesenchymal Stem Cell (MSC)-Derived Exosomes’, Journal of Clinical Medicine, 10(4), p. 711. Available at: https://doi.org/10.3390/jcm10040711.
[28] : Silva, A.K.A. et al. (2021) ‘Development of extracellular vesicle-based medicinal products: A position paper of the group “Extracellular Vesicle translatiOn to clinicaL perspectiVEs – EVOLVE France”’, Advanced Drug Delivery Reviews, 179, p. 114001. Available at: https://doi.org/10.1016/j.addr.2021.114001.
[17] : Luan, X. et al. (2017) ‘Engineering exosomes as refined biological nanoplatforms for drug delivery’, Acta Pharmacologica Sinica, 38(6), pp. 754–763. Available at: https://doi.org/10.1038/aps.2017.12.